A new CDC report highlights a dramatic increase in drug-resistant bacteria, posing a serious threat to public health.
Story Snapshot
- 20% surge in antimicrobial-resistant infections during the COVID-19 pandemic.
- *Candida auris* cases increased nearly five-fold from 2019 to 2022.
- CDC warns the rise threatens previous public health progress.
- Enhanced infection control and antibiotic stewardship are urgently needed.
Rising Threat of Drug-Resistant Bacteria
The CDC’s latest report documents a 20% increase in hospital-onset antimicrobial-resistant infections during the COVID-19 pandemic. The report underscores the pandemic’s detrimental impact on infection control and the heightened use of antibiotics. Among the alarming findings is the surge in *Candida auris* cases, which rose nearly five-fold from 2019 to 2022. This trend threatens the strides made in combating antimicrobial resistance and calls for immediate action to bolster infection control and stewardship programs.
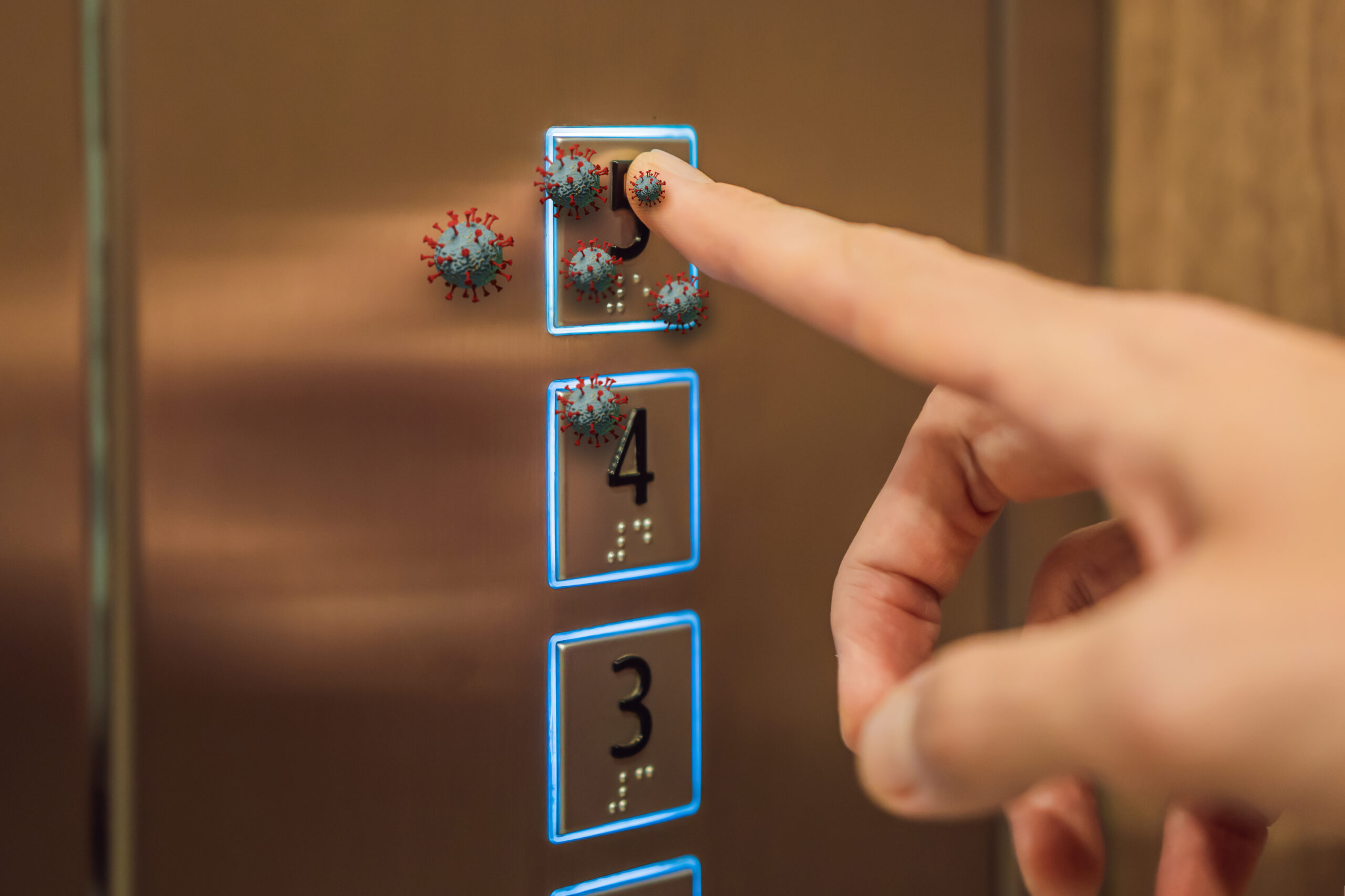
The emergence of superbugs is not a new phenomenon. Antimicrobial resistance has evolved over decades, accelerated by the overuse and misuse of antibiotics in medicine and agriculture. The COVID-19 pandemic further exacerbated the problem, leading to increased antibiotic prescriptions and strained healthcare resources, providing a fertile ground for drug-resistant bacteria to thrive.
The Impact of the Pandemic
The pandemic profoundly disrupted infection prevention efforts in healthcare settings, contributing to the rise in drug-resistant infections. The CDC’s report highlights a significant setback in controlling these infections, which were previously on a declining trend. Healthcare systems faced immense pressure, and measures that once curbed the spread of resistant bacteria were deprioritized, leading to the current crisis.
Experts emphasize that hospital-onset infections have particularly surged, with healthcare facilities struggling to maintain rigorous infection control protocols amid the pandemic’s demands. This environment allowed pathogens like *Candida auris* to spread more rapidly, showcasing the critical need for reinforced infection control measures.
The Economic and Public Health Implications
The economic burden of drug-resistant infections is staggering, with estimates suggesting an annual cost exceeding $4.6 billion in the U.S. alone for six key pathogens. Beyond the financial impact, the rise in resistant infections poses a grave threat to modern medicine’s effectiveness. Common procedures and treatments, such as surgeries and cancer therapies, become riskier without effective antibiotics, underscoring the urgency of addressing this issue.
The CDC’s report serves as a wake-up call for renewed efforts in infection control and antibiotic stewardship. Public health experts advocate for increased funding and global cooperation to combat the spread of superbugs. Strengthening surveillance and reporting systems is crucial, as is investing in the development of new antibiotics and diagnostic tools.
Looking Forward: Global Cooperation and Innovation
The rise of drug-resistant infections calls for a concerted global effort. Collaborative approaches involving healthcare providers, public health agencies, the pharmaceutical industry, and policymakers are essential to curb the spread of superbugs. Innovations in antibiotic development and diagnostic technology are vital to staying ahead of evolving pathogens.
Public awareness and education also play a critical role. Reducing unnecessary antibiotic use and promoting preventive measures can significantly impact the fight against antimicrobial resistance. The CDC’s findings highlight the pressing need for comprehensive strategies to safeguard public health and ensure the continued effectiveness of life-saving antibiotics.
Sources:
CDC Antimicrobial Resistance Facts and Stats
CDC About Antimicrobial Resistance
CDC Reports 70% Surge in Drug-Resistant “Nightmare Bacteria” Infections