Mississippi’s groundbreaking decision to cover expensive weight-loss drugs through Medicaid has produced a stunning reality check: only 2% of eligible adults have actually received prescriptions despite living in America’s second-most obese state.
Story Highlights
- Mississippi became one of only 13 states covering GLP-1 weight-loss drugs through Medicaid in 2023
- Despite 40% adult obesity rates, only 2,900 enrollees received treatment in the first 15 months
- State spent $12 million for 2,200 adult members, with nearly 90% being female patients
- Drug shortages, strict prior authorization, and limited provider awareness created significant barriers
- Highest-need areas like the Mississippi Delta saw the lowest utilization rates
A Promising Policy Meets Harsh Reality
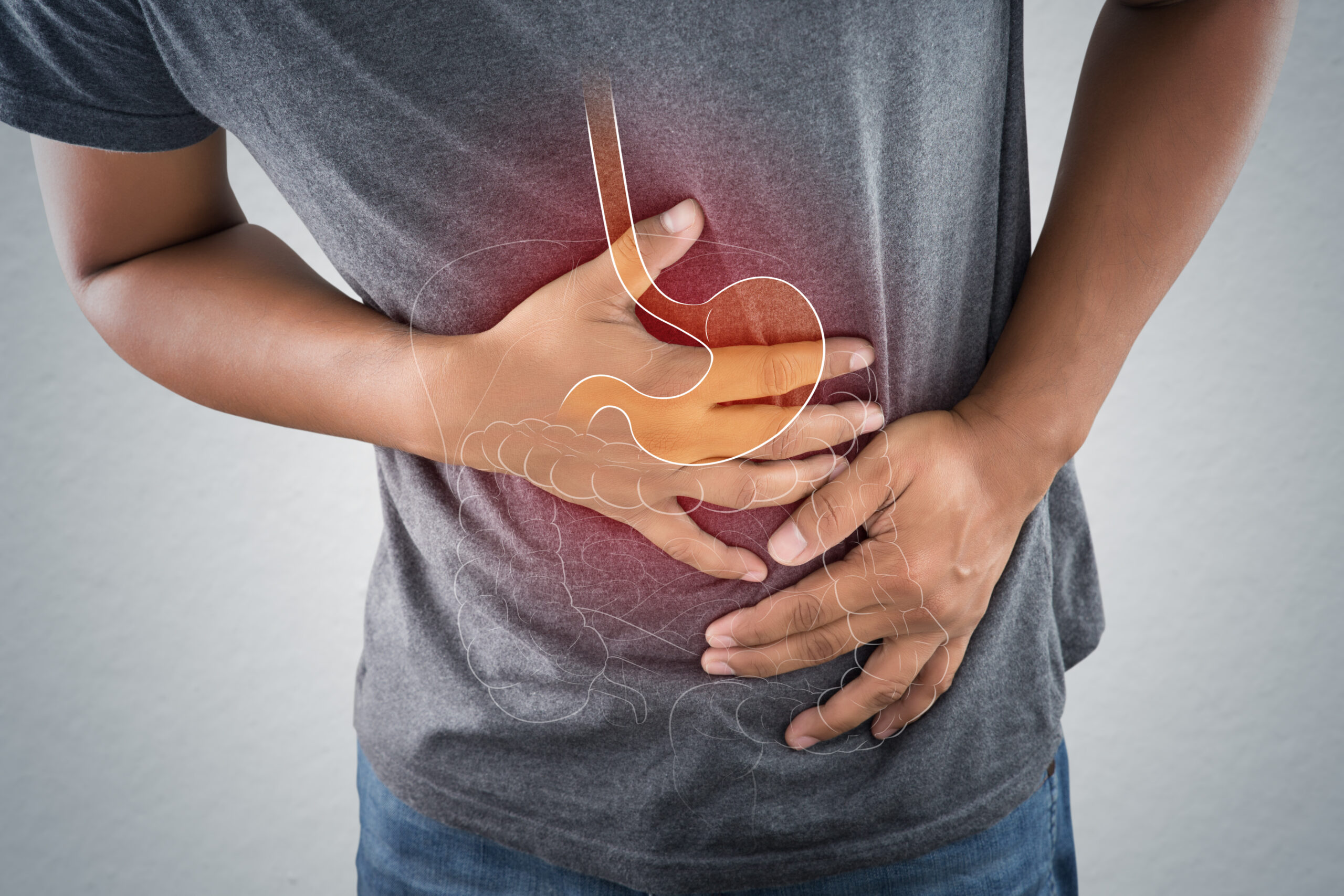
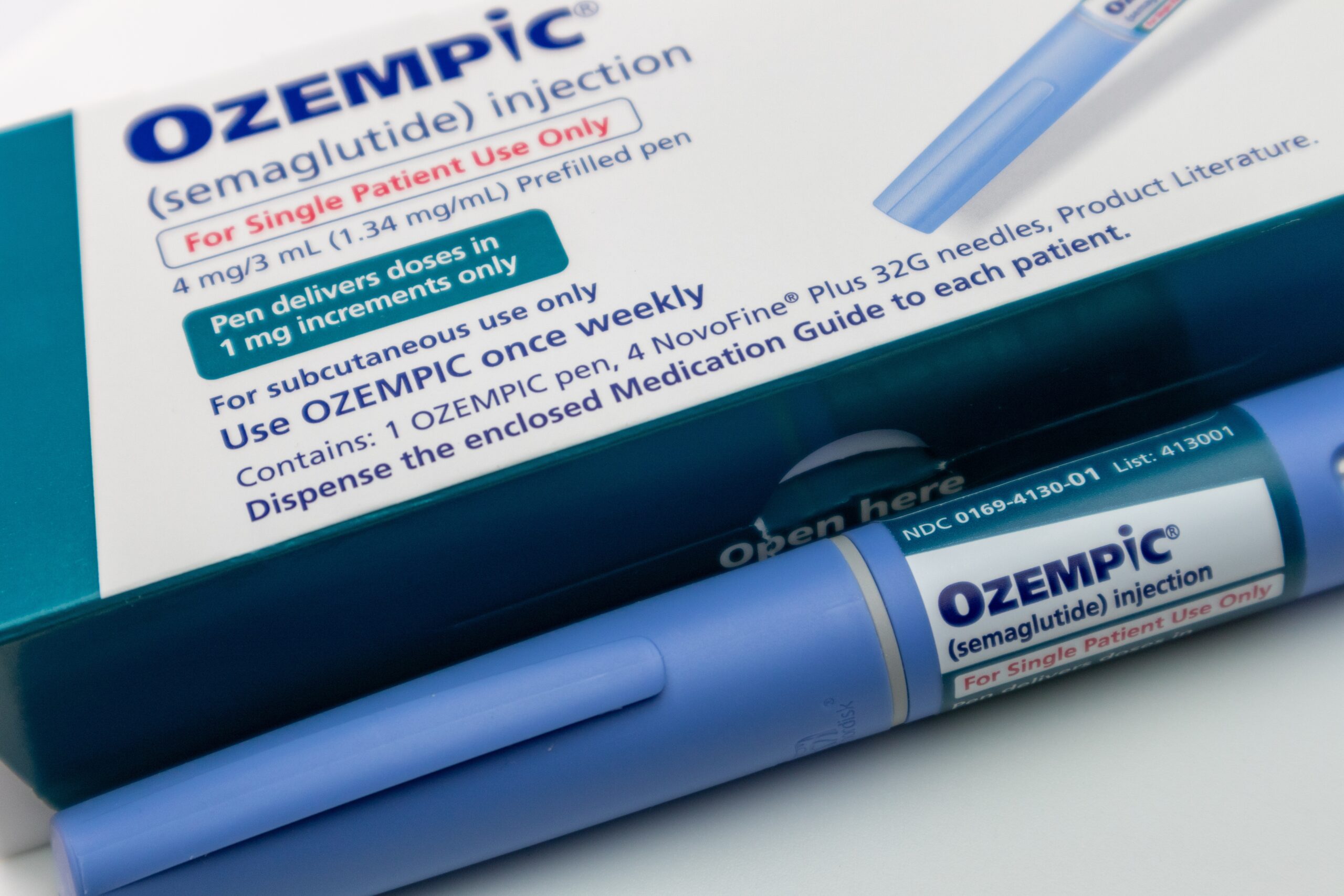
Mississippi Medicaid officials launched their GLP-1 coverage program with high hopes in 2023. The decision seemed logical for a state where obesity affects two out of every five adults and related health complications drain public resources. These drugs, including Wegovy and Saxenda, had proven remarkably effective in clinical trials, helping patients lose substantial weight when combined with lifestyle changes.
The math appeared straightforward: invest in expensive medications upfront to prevent costlier complications like diabetes, heart disease, and stroke later. Yet the program’s actual performance tells a different story entirely. With roughly 145,000 adults potentially eligible for these treatments, the 2% uptake rate represents a fraction of what policymakers anticipated.
In Mississippi, Medicaid Coverage of Weight Loss Drugs Fails to Catch On https://t.co/22m5Prtb3q
— Patty 🌻🇺🇸🌵 (@littlebytesnews) October 15, 2025
Barriers Create an Obstacle Course for Patients
Three primary factors have conspired to limit access despite official coverage. Drug shortages plague the entire GLP-1 market, with manufacturers struggling to meet surging national demand. Patients who manage to get prescribed often wait months for their medications, if they receive them at all.
Mississippi’s prior authorization requirements add another layer of complexity. Patients must demonstrate previous weight-loss attempts, meet specific BMI thresholds, and navigate administrative reviews before approval. Healthcare providers report spending excessive time on paperwork rather than patient care, discouraging many from prescribing these medications routinely.
In Mississippi, Medicaid Coverage of Weight Loss Drugs Fails To Catch On – KFF Health News https://t.co/D2s7EgqDbu
— Neil Floch MD (@NeilFlochMD) October 16, 2025
Geographic Disparities Reveal Deeper Problems
The program’s geographic distribution exposes troubling patterns about healthcare access in Mississippi. The Delta region, which suffers from the state’s highest obesity rates and poorest health outcomes, shows the lowest utilization of these new treatments. Rural areas lack specialists familiar with GLP-1 protocols, and many primary care providers remain unaware of the coverage changes.
This disparity undermines the program’s potential to address health inequities. The patients who most need these interventions live in areas with the least capacity to deliver them effectively. Urban centers near Jackson and the Gulf Coast account for most prescriptions, while Delta communities continue struggling with limited options.
Financial Implications Raise Long-Term Questions
Mississippi’s $12 million expenditure over 15 months represents significant per-patient costs averaging roughly $5,500 annually per adult member. These figures will likely increase if utilization grows, raising questions about budget sustainability. State officials must balance expanding access with controlling costs, particularly given Mississippi’s historically conservative approach to Medicaid spending.
The program’s future depends largely on demonstrating measurable health improvements and eventual cost savings through reduced obesity-related complications. Early results show promise for individual patients, but population-level impacts remain unclear given the limited uptake. Policymakers need substantial data proving long-term value to justify continued investment in these expensive treatments.
Sources:
In Mississippi, Medicaid Coverage of Weight Loss Drugs Fails to Catch On – KFF Health News
Medicaid Coverage of and Spending on GLP-1s – KFF
Medicaid Coverage for Weight Loss Drugs – GoodRx
Mississippi Medicaid Anti-obesity Select Agents PA Criteria