A new experimental drug pairing is shaking up the fight against aggressive ovarian cancer, offering hope for patients—and exposing just how much was squandered when the previous administration chose bureaucracy over breakthroughs.
At a Glance
- Researchers are using CRISPR gene-editing and innovative drug pairings to tackle drug-resistant ovarian cancer.
- Clinical trials show experimental therapies may increase survival rates for women with aggressive disease.
- FDA has granted Regenerative Medicine Advanced Therapy (RMAT) designation to a leading cell therapy, fast-tracking its review.
- Ongoing studies could pave the way for personalized cancer treatments and wider use of gene-editing technology in oncology.
Experimental Drug Pairing Targets Deadly Ovarian Cancer
Researchers across the country are charging full steam ahead with new therapies for ovarian cancer, a disease that has been a death sentence for far too many women for far too long. The latest approach combines gene-editing—yes, the same CRISPR technology that once had progressives wringing their hands over “ethics”—with advanced drug delivery systems and cell therapies. The goal: outsmart the cancer’s notorious ability to resist standard treatments, and finally give patients a fighting chance.
📢Paper by #ListerFellow Marco di Antonio et al. from @imperialcollege. Targeting four-stranded DNA structures (G-quadruplexes) could reverse chemoresistance in ovarian cancer.
🔗https://t.co/opONZl7qLY pic.twitter.com/9jrAbm5p66— The Lister Institute of Preventive Medicine (@ListerInstitute) July 14, 2025
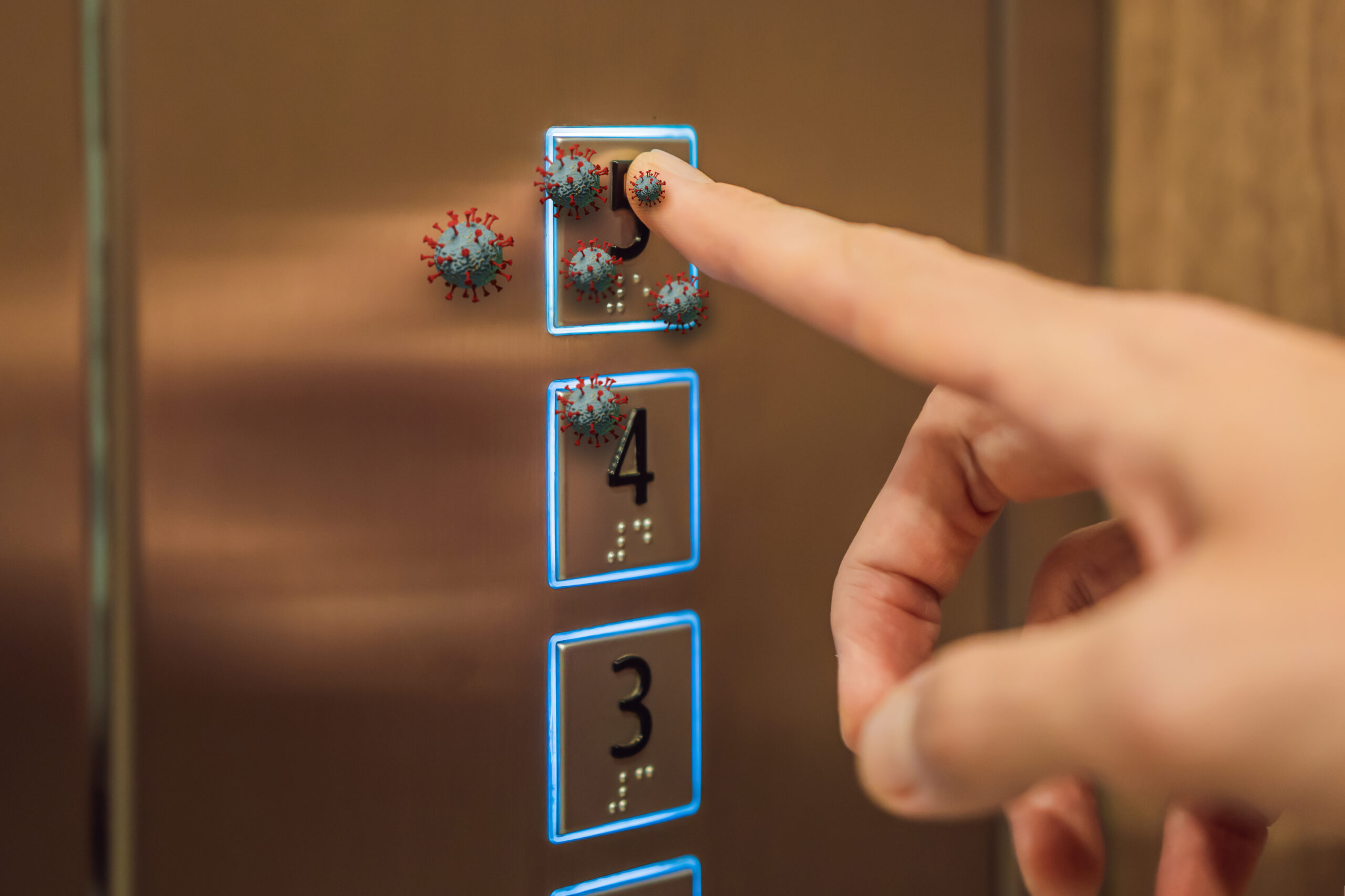
The backbone of this fight is CRISPR/Cas9 gene-editing, a tool now being used to identify and target genes that help ovarian cancer survive and bounce back after chemo. Add to that a peptide inhibitor targeting the CBX2 protein—which is linked to chemo resistance—and you have a one-two punch in the lab that’s already showing promise in animal models. Meanwhile, cell therapy approaches like Vigil are moving through clinical trials, with recent results suggesting a meaningful boost in survival for women with the deadliest forms of the disease. And unlike the endless government programs of the past, these innovations are being fast-tracked: the FDA gave RMAT designation to Vigil, signaling that the agency finally recognizes the urgency and potential of these therapies.
Watch a report: CRISPR Breakthroughs: Revolutionizing Genome Editing
Clinical Trial Progress Brings Renewed Hope for Patients
The numbers are sobering: ovarian cancer claims nearly 13,000 American lives every year, most of them diagnosed too late for standard treatment to make a dent. For years, women and their families have been left with little more than platitudes and pink ribbons—while bureaucrats debated, and funding dried up for anything that threatened the status quo. But the tide is turning in 2025, as multiple clinical trials ramp up for CRISPR-based therapies, nano-delivery drug pairings, and next-generation immunotherapies.
The VITAL phase 2b trial for Vigil immunotherapy is expected to wrap up by the end of this year, and early data is strong: for certain high-risk subtypes, survival rates are up, and side effects are down compared to the old chemo regimens. At least 150 gene-editing clinical trials are active worldwide, and researchers are optimistic that these approaches could soon break the cycle of recurrence and resistance that has plagued ovarian cancer treatment for decades. The science is moving fast—and for a change, the regulators are keeping up.
From Lab to Bedside: America Leads in Cancer Innovation
America’s research labs are once again the envy of the world, as teams from top universities and biotech firms drive the development of these experimental therapies. It’s not just scientists in white coats who care, either—patients and advocacy groups are demanding access to trials, and clinicians are eager for better tools in the fight against this brutal disease. The economic impact could be massive: if these therapies prove effective, the long-term savings in healthcare costs will dwarf the upfront investment, and families will be spared the heartbreak and financial ruin that comes with late-stage cancer.
Of course, there are still challenges. Some experts are urging caution about the long-term safety of gene-editing and the ethics of personalized medicine. But after years of government dithering and wasted time, the message from the lab is clear: with the right tools and a government that prioritizes innovation over red tape, American patients can—and should—expect cures, not just treatments.