One man’s excruciating back pain led to a misdiagnosis of schizophrenia, all because a common painkiller quietly unleashed vivid hallucinations—and the true culprit almost slipped past doctors unnoticed.
Story Snapshot
- Norco, a widely used opioid, can trigger hallucinations that mimic severe psychiatric disorders.
- A patient’s experience exposed how easily these symptoms are misattributed, leading to a schizophrenia misdiagnosis.
- Doctors warn that opioid-induced hallucinations remain underreported and often mistaken for mental illness.
- Even prescribed doses can cause dangerous neurotoxic effects, especially in older adults.
Common Painkillers Can Cause Psychiatric Chaos
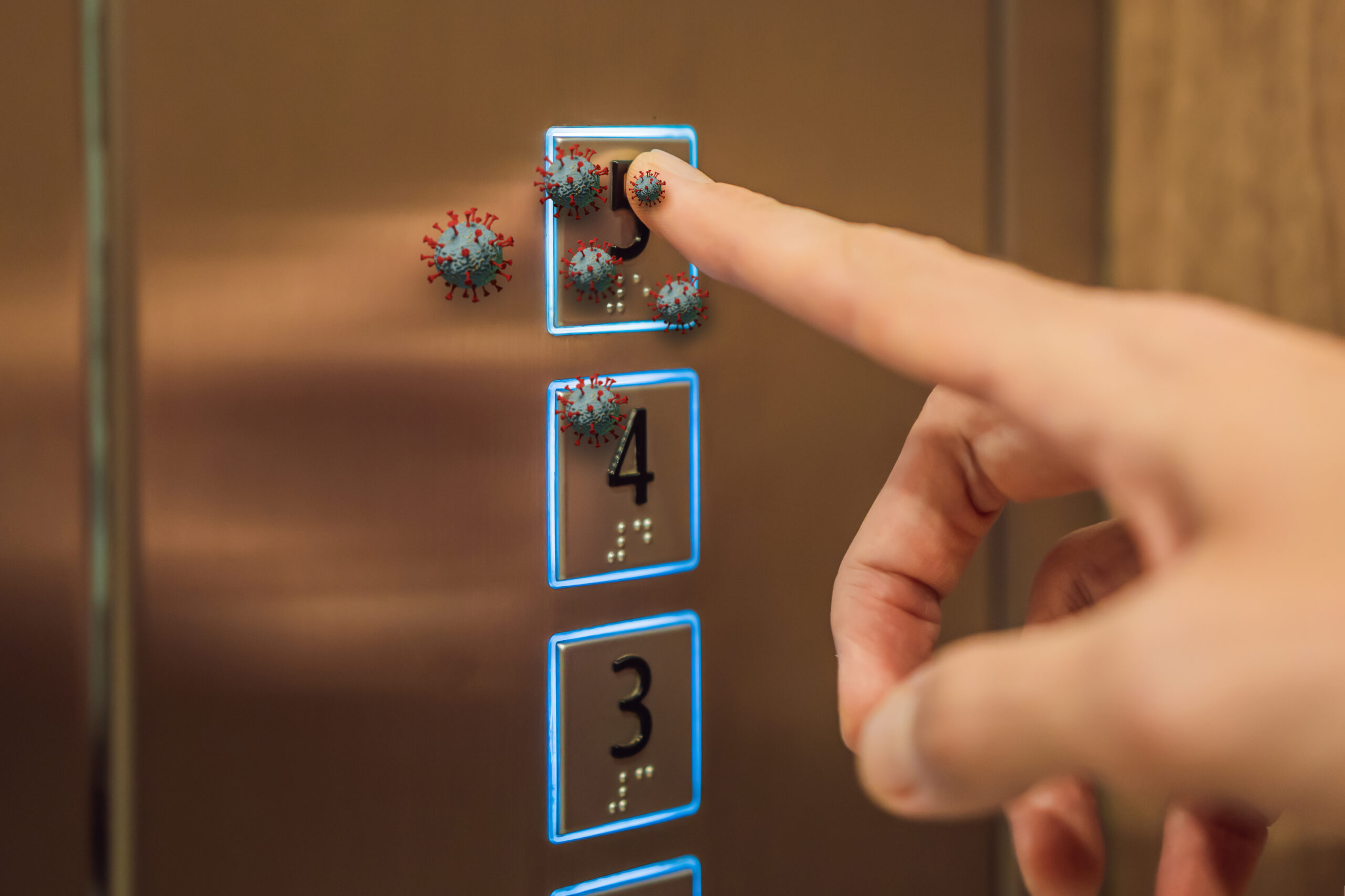
Norco—a familiar name in medicine cabinets across America—promises relief from the relentless grip of chronic pain. Its active ingredients, hydrocodone and acetaminophen, are trusted by millions and even prescribed for nagging coughs or persistent diarrhea. Yet, behind the comfort of its daily use, a shadow lurks: Norco can trigger vivid auditory and visual hallucinations, a side effect so rarely reported that most healthcare providers may never suspect it. The true danger comes not just from the hallucinations themselves, but from how easily they can be mistaken for symptoms of mental illness, setting patients down a path of unnecessary psychiatric treatment.
Doctors at Louisiana State University Health Sciences Centre detailed the case of a 67-year-old man from Shreveport, Louisiana. Two years after a seizure, he found himself haunted by terrifying visions—people attacking him, animals lurking where none existed. The diagnosis? Schizophrenia. He was prescribed antipsychotics, which dulled the hallucinations but never truly banished them. His family history showed no trace of mental illness, and his symptoms began well past the age when schizophrenia typically emerges. Only when he increased his Norco dosage for worsening back pain did the hallucinations intensify to an unbearable degree. The correlation between dose and symptom severity became impossible to ignore.
Opioid Neurotoxicity Often Hides in Plain Sight
Withdrawal from Norco marked a dramatic turning point. The hallucinations vanished without a trace, and paranoia dissolved. Doctors reviewing his case highlighted a critical oversight in clinical practice: vivid hallucinations in older adults, especially those with no history of mental health disorders, should trigger suspicion of alternative causes beyond psychiatric disease. The medical literature describes opioid-induced hallucinations as underreported and frequently misattributed. Studies confirm that higher doses of opioids increase the risk of neurotoxic effects—including hallucinations—yet most physicians remain unaware of this risk. The opioid epidemic’s familiar warnings about addiction and overdose have overshadowed these subtler, insidious side effects.
The patient’s other risk factors—chronic disease, advanced age, and a history of seizures—complicated the picture. Seizure clusters can themselves provoke confusion and hallucinations, but the timing and escalation of his symptoms traced neatly to his use of Norco. Cannabis, which he used occasionally, was ruled out as a cause; research shows it rarely drives full-blown psychosis in adults. The lesson: in older patients, sudden psychiatric symptoms often have a medical explanation hiding in plain sight.
Long-term Opioid Use: A Prescription for Dependence and Diagnostic Confusion
Health officials in the United States and United Kingdom have long cautioned against prolonged opioid use. The U.S. Food and Drug Administration warns that Norco exposes patients to the risk of addiction, overdose, and death. Beyond these headline dangers, high-dose opioids are now recognized as likely to spark neurotoxic reactions, including hallucinations, agitation, and confusion. Despite these warnings, prescriptions for potent painkillers have surged since the pandemic, as routine medical care delays pushed more patients toward pharmaceutical relief. Research found a 40 percent jump in opioid prescribing after lockdowns, fueling concerns that dependence is becoming a new normal—sometimes with devastating consequences far beyond addiction alone.
Schizophrenia affects roughly 1 percent of the world’s population, with most cases appearing between the ages of 16 and 30. The sudden onset of paranoia and hallucinations in older adults, especially without family history or previous mental illness, should always raise red flags for alternative causes. The misdiagnosis in this man’s case underscores the need for vigilance: doctors and patients alike must recognize that not all hallucinations are psychiatric in origin. Sometimes, the true culprit is hiding in the medicine cabinet.
Sources: