What if your eco-friendly menstrual cup could quietly sabotage your birth control—without you ever realizing it?
Story Snapshot
- French study links menstrual cup use to a 2.6–3.1x higher risk of IUD displacement
- Most affected: young, urban women with copper IUDs
- Clinics now directly counsel patients on menstrual cup risks and safe removal
- Mechanism remains unclear, but clinical guidelines may soon evolve
Menstrual Cups and IUDs: A Collision of Good Intentions
Menstrual cups and intrauterine devices (IUDs) are two modern marvels of women’s health—each touted for freedom, convenience, and control. Yet, as Parisian clinicians discovered, combining these two innovations can trigger consequences that few expected. The latest French study, led by Dr. Roxane Liard and Dr. Hervé Picard, found menstrual cup users face more than double the risk of IUD displacement. When eco-conscious hygiene meets long-acting contraception, the result may be a hidden hazard that upends the very autonomy women seek.
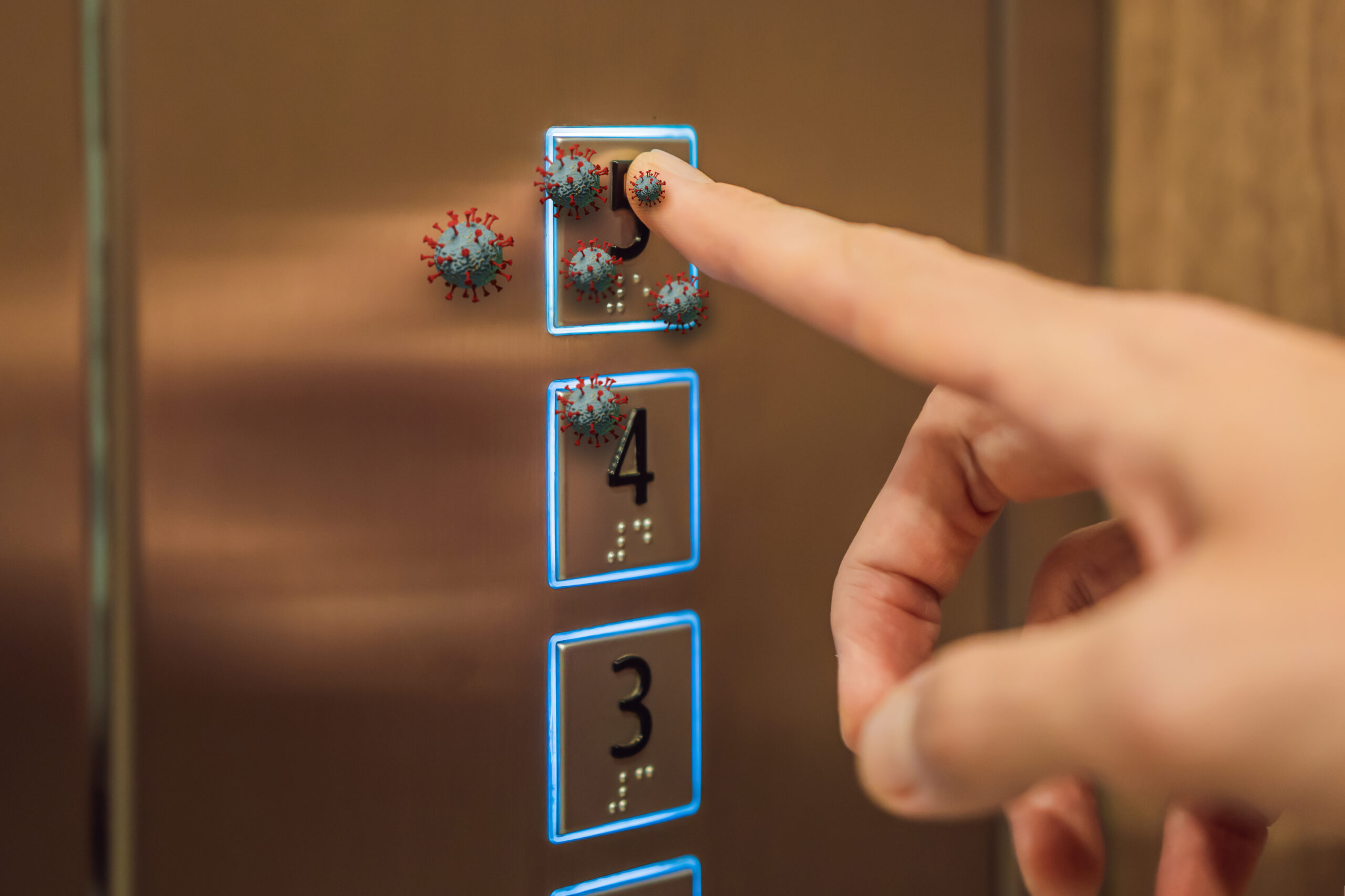
IUD displacement isn’t just a technical hiccup. Even a minor shift can spell contraceptive failure, unexpected pregnancy, or sudden pain. The French research, enrolling 747 women from March 2020 to May 2021 in Paris, relied on ultrasound precision to confirm every IUD’s position. Adjusting for known risk factors—device type, prior expulsions, BMI, and more—the study established a clear pattern: menstrual cup users experienced a 2.6–3.1-fold increase in IUD displacement events compared to non-users. The effect was especially pronounced among copper IUD users, who faced a fourfold risk compared to hormonal IUD users.
Why Has No One Sounded the Alarm Before?
Prior research failed to settle the debate, often mired in small sample sizes, retrospective surveys, or lack of ultrasound confirmation. The D-COUPE study suggested a fourfold increased risk, but critics flagged its design flaws. Some academic voices claimed there was no link, but their evidence could not withstand scrutiny. The CUP-DIU study, published in May 2025, stands apart for its rigorous prospective approach and transparent adjustment for confounders. The Paris clinics, serving a young, urban, mostly nulliparous population, became a bellwether for a problem likely playing out in cities across the developed world.
French clinicians first noticed the pattern: women returning for routine IUD checks after switching to menstrual cups sometimes presented with a displaced or expelled device. These observations, initially anecdotal, drove the research team to systematically examine the phenomenon. Their findings are now reshaping contraceptive counseling and menstrual health education in real time.
Clinical Practice in Flux: New Rules for Safe Menstrual Cup Use
Today, clinics in Paris and beyond have revised their scripts. Before placing an IUD, practitioners now ask about menstrual cup use. If the answer is yes, women receive targeted advice—break the suction seal before removal, pull from the stem instead of the base, and monitor for symptoms like pain or unexpected bleeding. Dr. Liard and her colleagues do not advocate abandoning menstrual cups. Instead, they urge vigilance: awareness of the risk and careful technique can minimize the chance of IUD displacement. Patients are counseled to report any warning signs, and follow-up ultrasounds are more common among high-risk users.
These practical changes reflect an embrace of patient autonomy. Rather than dictate bans or stoke fear, clinicians equip women with the knowledge to make informed choices—balancing environmental values against reproductive security. The shift signals a new era of shared decision-making in women’s health, where open dialogue trumps top-down mandates.
Unanswered Questions and the Road Ahead
No one yet knows the exact mechanism by which menstrual cups dislodge an IUD. Hypotheses abound: the cup’s suction, proximity to the cervix, or user technique may all play a role. The French study controlled for confounders like BMI and parity, but could not settle the “how.” Researchers and clinicians agree that more investigation is urgently needed, especially across diverse populations and device types. The findings already have ripple effects—guideline committees and professional societies may soon rewrite their recommendations, and menstrual cup manufacturers might need to rethink product warnings or design tweaks.
For now, women using both IUDs and menstrual cups occupy a gray zone: empowered by choice, yet exposed to a risk that only recently came to light. The next wave of research may pinpoint safer methods, but the lesson is clear—when medical innovation races ahead, only constant vigilance keeps autonomy from becoming vulnerability.
Sources:
Clinical Advisor: Menstrual cup use may increase the risk for IUD displacement
PMC: Menstrual cup use and IUD displacement—French cohort study